Breast Imaging
Breast cancer
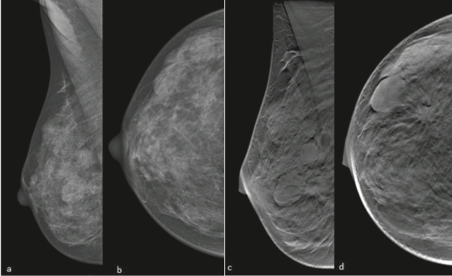
Breast cancer is the most common female invasive cancer in Western countries. It represents almost 25% of female cancers, affecting 1 in 10 women. In recent years, breast cancer mortality of under 49-year-old women decreased by almost 11% in Italy. This reduction demonstrates the relevance of early diagnosis through breast imaging in order to improve treatment strategies and outcomes. Digital breast tomosynthesis (DBT) is an emerging diagnostic technique which overcomes the 2-dimensional (2D) format limit of conventional digital mammography (DM) and provide a 3D reconstruction of the breast, minimizing the effect of overlapping breast tissue and improving the detection of any lesions especially in dense breast [Fig 1].
| Fig.1 39 y-o woman. a, b Digital mammography (mediolateral oblique (MLO) and craniocaudal (CC) views) showing a dense breast (ACR d) with circumscribed and benign-appearing masses (BI-RADS 3); c, d Digital breast tomosynthesis (MLO and CC views) clearly showing a spiculated mass (BI-RADS 5); surgical pathology confirmed invasive ductal carcinoma. |
A newer diagnostic tool to improve DM diagnostic performance is Contrast enhanced spectral mammography (CESM). CESM is an innovative and clinically useful method for breast assessment based on injection of an iodinated intra-venous contrast agent. Similar to Magnetic Resonance Imaging (MRI), CESM shows abnormal enhancement of neoplastic tissue compared to surrounding breast tissue. Future research and prospective clinical trials are necessary to validate this promising technique and define its field of use among breast imaging indications. To date the value of MRI as the most sensible technique in breast imaging is well-established. Dynamic contrast-enhanced MRI plays a pivotal role in the clinical setting, and its indications, from locoregional staging [Fig 2] to neoadjuvant therapy response evaluation, are widely recognized.

| Fig.2 50 y-o woman with multicentric disease (IDC). T1 fat-saturated contrast-enhanced sagittal breast MRI clearly identifies four lesions on left breast (a,b), corresponding to four spiculated masses (c, d (circles)) on MLO DBT projections. MRI and DBT obtained good correlation in terms of lesions number and tumor size. Histologic evaluation showed multiple foci of invasive ductal carcinoma (e). |
Nevertheless, even with the spread of 3 T scanners, breast MRI specificity is still variable, ranging between 72 and 94%, so functional techniques, such as MR spectroscopy [Fig 3] and diffusion-weighted imaging (DWI) [Fig 4], have been widely investigated to increase breast MRI diagnostic accuracy and to provide biomarker information. New perspective of breast MRI imaging are artificial intelligence tools such as radiomics and radiogenomis, whose final purpose is to create non-invasive biomarkers able to predict breast cancer risk and outcomes. In conclusion, the integration of functional techniques and artificial intelligence in the clinical setting allows to personalize treatment and management, as is essential in the precision medicine era.


| Fig.3 A–F, 55-year-old patient, IDC, ER 60%, PgR 80%, Her2+, nuclear grade 3, Ki-67 50%. A, IDEAL water-only T2-weighted sequence on axial plane: high signal mass-like lesion. B, VIBRANT T1-weighted sequence after contrast agent administration: the lesion shows irregular margins and it is associated with nipple and skin retraction. C, Subtracted T1-weighted image on axial plane. Lesion size is 33 mm. D, Perfusion color map confirms the mass lesion on the left breast. E, Volume of interest with side bands on axial plane and single-voxel spectrum,(F) which shows choline (Cho)resonance peak at 3.22 ppm |
| Fig.4 A-D, 57-year-old patient, IDC. A, CC DBT view showing an architectural distortion in the right OUQ; B, axial subtracted T1 weighted post-contrast (DCE) image showing a 35 mm non-mass lesion in the right OUQ; C, axial IDEAL water-only T2-weighted sequence: high signal non-mass lesion; D, axial DWI image (b-1000) shows a 35 mm area of hyperintensity. |
References
1. Added value of digital breast tomosynthesis combined with digital mammography according to reader agreement: changes in BIRADS rate and follow-up management. Galati F., Marzocca F., Bassetti E., Luciani M.L., Tan S., Catalano C., Pediconi F. - Breast Care 2017 Sep ; 12 (4) :218-222. DOI: 10.1159/000477537
2. Preoperative Staging in Women with Known Breast Cancer: Comparison between Digital Breast Tomosynthesis (DBT) and Magnetic Resonance Imaging (MRI). Galati F., Marzocca F., Tancredi A., Collalunga E., Catalano C., Pediconi F. - Cancer and Clinical Oncology 2018; Vol. 7, No. 2: 33-42; DOI:10.5539/cco.v7n2p33
3. Can unenhanced MRI of the breast replace contrast-enhanced MRI in assessing response to neoadjuvant chemotherapy? Cavallo Marincola B., Telesca M., Zaccagna F., Riemer F., Anzidei M., Catalano C., Pediconi F. - Acta Radiologica 2019, Vol. 60(1) 35–44 DOI: 10.1177/0284185118773512
4. Peritumoral edema as a biomarker of the aggressiveness of breast cancer: results of a retrospective study on a 3 T scanner. Panzironi G., Moffa G., Galati F., Marzocca F., Rizzo V., Pediconi F. - Breast Cancer Res Treat. 2020 May;181(1):53-60. doi: 10.1007/s10549-020-05592-8
5. Breast Magnetic Resonance Spectroscopy at 3 T in Biopsy-Proven Breast Cancers: Does Choline Peak Correlate With Prognostic Factors? Galati F., Luciani M.L., Caramanico C., Moffa G., Catalano C., Pediconi F. - Invest Radiol. 2019 Dec;54(12):767-773. doi: 10.1097/RLI.0000000000000597.PMID: 31356383