
Genitourinary
Prostate
Prostate cancer is the most prevalent tumor in males, and early diagnosis is essential in order to reduce its morbidity and mortality. However, the conventional screening method based on serum PSA dosage and systematic (random) biopsies has proved to be highly inefficient and imprecise.
A more appropriate diagnostic work-up, leveraging state-of-the-art medical imaging technologies, would be one based on multiparametric MRI(mpMRI) and MRI-targeted biopsy.
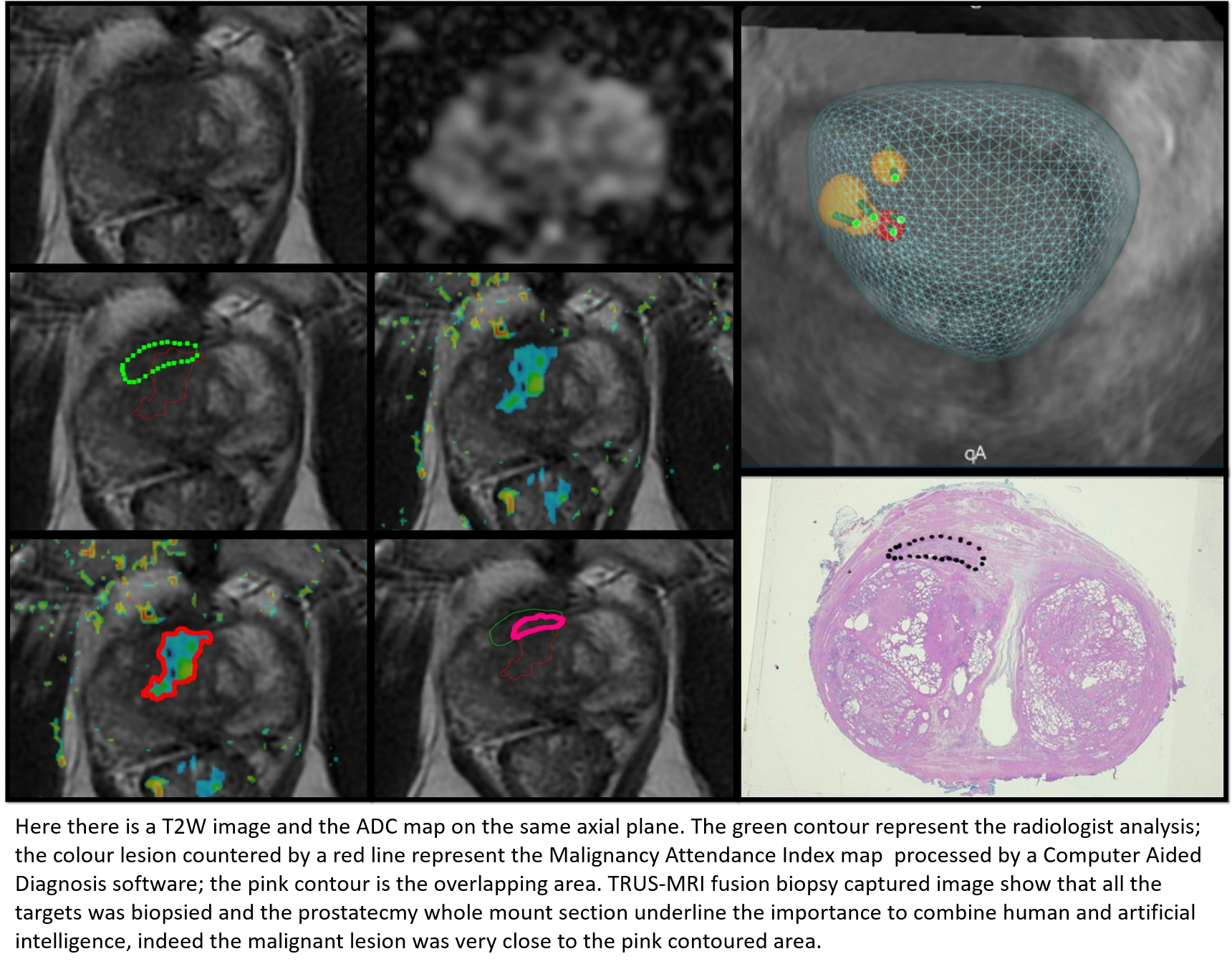
Multiparametric MRI of the prostate is a highly accurate diagnostic tool holding very high negative and positive predictive values, capable to identify the vast majority of clinically significant cancers while at the same time avoiding overdiagnosis of indolent disease that would not require treatment. Not only is mpMRI a highly accurate diagnostic modality, but it also allows us to target bioptic sampling of the suspicious foci (MRI-targeted biopsy), consequently limiting the invasiveness and the morbidity of conventional random biopsy, maximizing detection rate and minimizing overdiagnosis.

At our institution we are fully committed in the advancement of the so-called MRI pathway for prostate cancer diagnosis, both from the point of view of research activity, knowledge dissemination and delivery of healthcare.
Bladder
In addition to early diagnosis, precision medicine in oncology requires us to accurately characterize and classify disease phenotypes so that the right treatment can be specifically delivered to the right patient.
One research and clinical field of application we are currently deeply involved in is the use of multiparametric MRI of the bladder to more accurately and non-invasively characterize bladder lesions.
Bladder cancer comprises two pathologically and clinically different entities: muscle-invasive bladder cancer, which requires radical cystectomy, and non muscle-invasive bladder cancer, usually requiring only trans-urethral resection (TUR). The use of mpMRI of the bladder, consisting of a well-defined and standardized imaging acquisition protocol, to classify bladder cancer allows a more precise and less invasive diagnostic workup compared to conventional diagnostic TUR.
References
1. Panebianco V, Pecoraro M, Fiscon G, Paci P, Farina L, Catalano C. Prostate cancer screening research can benefit from network medicine: an emerging awareness. npj Systems Biology and Applications 2020;6(1):13.
2. Kasivisvanathan V, Rannikko AS, Borghi M, et al. MRI-Targeted or Standard Biopsy for Prostate-Cancer Diagnosis. N Engl J Med 2018;378(19):1767–77.
3. Panebianco V, Barchetti G, Simone G, et al. Negative Multiparametric Magnetic Resonance Imaging for Prostate Cancer: What’s Next? European Urology 2018;74(1):48–54.
4. Panebianco V, Barchetti F, Sciarra A, et al. Multiparametric magnetic resonance imaging vs. standard care in men being evaluated for prostate cancer: A randomized study. Urologic Oncology: Seminars and Original Investigations 2015;33(1):17.e1-17.e7.
5. Panebianco V, Narumi Y, Altun E, et al. Multiparametric Magnetic Resonance Imaging for Bladder Cancer: Development of VI-RADS (Vesical Imaging-Reporting And Data System). European Urology 2018;74(3):294–306.
6. Del Giudice F, Barchetti G, De Berardinis E, et al. Prospective Assessment of Vesical Imaging Reporting and Data System (VI-RADS) and Its Clinical Impact on the Management of High-risk Non–muscle-invasive Bladder Cancer Patients Candidate for Repeated Transurethral Resection. European Urology 2020;77(1):101–9.

